Lidocaine Hydrochloride Injection 2.5%
Contents of the pack and other information
What Lidocaine Injection contains
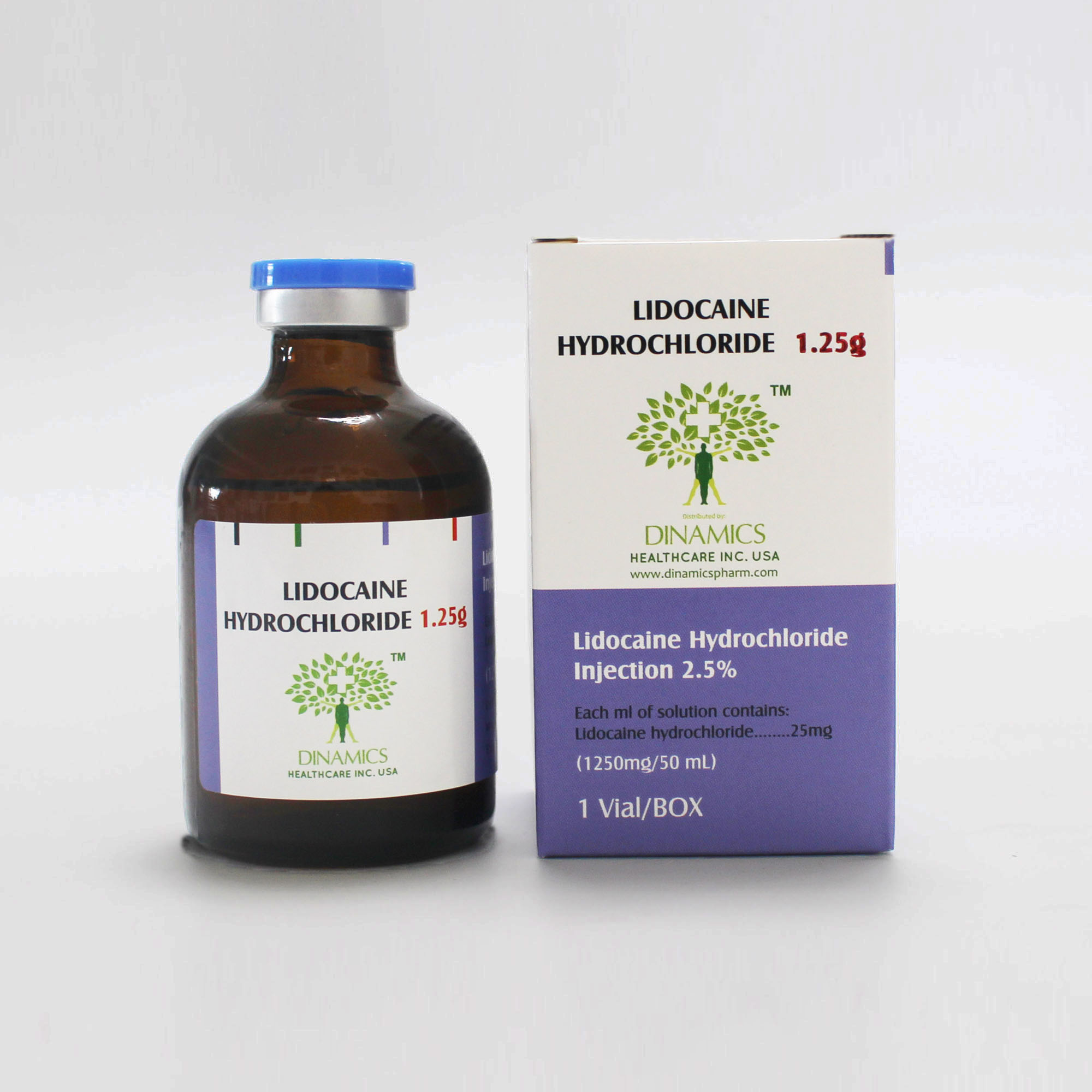
•The active substance is lidocaine hydrochloride. Each ml contains 25 mg of lidocaine hydrochloride.
What Lidocaine Injection looks like and contents of the pack
•Lidocaine injection is a clear, sterile, nonpyrogenic solution, free from visible particles. It is supplied in a 50-mL glass vial.
•Pack size:
1 vial per carton.
DESCRIPTION
1. What Lidocaine Injection is and what it is used for
Lidocaine injection is a sterile, nonpyrogenic solution available in the concentration of 2.5% (m/v). Lidocaine injection is used to treat:
-Nerve block anaesthesia.
-Severe symptomatic ventricular tachycardia if judged to be life-threatening by the doctor.
2. What you need to know before you take Lidocaine Injection
2.5% w/v Lidocaine Injection must not be used in cases of:
- Severely disturbed cardiac conduction (sinu-atrial, atrioventricular or intraventricular blocks of higher degree, e.g. 2nd and 3rd degree A-V block),
- Use during the first three months after myocardial infarction or in conditions of reduced cardiac output (left ventricular output less than 35 per cent of normal),
- Bradycardia with heart rate below 50 BPM. - ADAMS-STOKES Syndrome
- WOLFF-PARKINSON-WHITE Syndrome,
- Hypersensitivity to amide-type local anaesthetics,
- Suspicion of hereditary tendency to malignant hyperthermia,
Additionally, in nerve block anaesthetics, 2.5% w/v Lidocaine Injection BP must not be used in the following conditions: - Disorders of blood coagulation, anticoagulant therapy,
- Infections in the region of injection, - Uncooperative patient.
Special warnings
In narcotised patients central nervous disorders may remain unrecognised and cardiac side effects may suddenly occur.
During prolonged therapy with Lidocaine infusions water and electrolyte balance should be monitored.
Special precautions for use
Especially careful medical monitoring is mandatory if 2.5% w/v Lidocaine Injection BP is used in the following conditions: - Disorders of cardiac impulse generation and conduction (Sick Sinus Syndrome, 1st degree A-V block, Bundle Branch Block),
- Hypoxia,
- Respiratory depression,
- Increased tendency to convulsions, - Hypovolaemia,
- Shock,
- Diseases of liver and kidneys,
- Myocardial weakness (cardiac insufficiency),
- Severe hypotension (systolic blood pressure below 90 mm Hg).
Before undertaking any local anaesthetic procedure, venous access is recommended. Appropriate instruments and drugs for emergency treatment should be made available.
Taking other medicines
Beta blockers (e.g. propranolol, metoprolol), cimetidine, and noradrenaline have a synergetic effect on the action of
Lidocaine; in acidosis, the plasma concentration of free Lidocaine is increased. These conditions may necessitate dose reduction.
If 2.5% w/v Lidocaine Injection is combined with other anti-arrhythmic agents such as beta blockers or calcium antagonists, the inhibitory effect on cardiac conduction and contractility may be enhanced.
If 2.5% w/v Lidocaine Injection and inhalation narcotics are given simultaneously, there may be mutual synergisms regarding their depressive effects.
If epinephrine or noradrenaline are given additionally, but separately, frequency or seriousness of side effects on the heart may be markedly increased.
Drugs stimulating the hepatic metabolism of drug substances by microsomal enzyme induction, e.g. phenobarbital or phenytoin, reduce the efficacy of Lidocaine.
Lidocaine may have a synergetic effect on peripheral muscle relaxants, especially suxamethonium chloride.
Simultaneously administered diazepam raises the threshold for Lidocaine to produce convulsions. This must be kept in mind when monitoring patients for signs of toxicity of Lidocaine.
Pregnancy and lactation
Lidocaine crosses the placental barrier. During pregnancy, 2.5% w/v Lidocaine Injection should only be used if the expected benefits clearly outweigh potential hazards. The doses applied should be as low as possible. 2.5% w/v Lidocaine
Injection should also be used very cautiously in obstetrics, especially in situations of foetal hypoxia and acidosis. Lidocaine is secreted into breast milk. Therefore, caution should be exercised when administering 2.5% w/v Lidocaine Injection to nursing women. In general, however, nursing does not have to be discontinued.
DIRECTION
1.How to take Lidocaine Injection
How is given
Nerve block anaesthesia
Intracutaneous, subcutaneous, intramuscular, perineural and epidural injection for nerve block anaesthesia. Antiarrhythmic therapy
Slow intravenous injection or Intravenous infusion after dilution with appropriate amounts of a suitable vehicle solution.
How much is given
Nerve block anaesthesia
Adults:
Unless directed otherwise, up to 200 mg of Lidocaine hydrochloride, corresponding to approx. 8 ml 2.5% w/v Lidocaine Injection, are given to adults.
The maximum daily dose is 200 mg of Lidocaine hydrochloride.
Children:
The dosage should be calculated in ml per kg body weight. Unless prescribed otherwise, children are administered up to 4 mg of Lidocaine hydrochloride, corresponding to approx. 0.16 ml of 2.5 % w/v Lidocaine Injection.
The maximum daily dose is 4 mg of Lidocaine hydrochloride per kg B.W.
When Lidocaine is used in obstetrics, it must be remembered that pregnant women need 1/3 less of local anaesthetics. The dose should be reduced in patients with heart failure, liver diseases, in patients receiving drugs which enhance the effects of Lidocaine and in patients who are more than 60 years old.
As a matter of principle, the lowest possible dose and concentration of the local anaesthetic should be used. Antiarrhythmic therapy
Adults:
Unless directed otherwise, initially 70-100 mg (1-1.5 mg/kg B.W.) of Lidocaine hydrochloride are injected slowly i.v. The maximum injection rate is 25 mg/min., corresponding to approx. 1.2 ml of 2.5 % w/v Lidocaine Injection per minute.
If the first injection is ineffective, a second dose - one third to half of the initial dose - may be injected after 5 - 10 minutes.
Within one hour, not more than 200 - 300 mg of Lidocaine hydrochloride should be given, corresponding to approx. 8.0 - 12.0 ml of 2.5 % w/v Lidocaine Injection.
For maintenance of therapeutic plasma levels of Lidocaine hydrochloride (1.5 - 5 μg/ml), Lidocaine hydrochloride is infused at a dose of 20 - 50 μg per kg BW per min, corresponding to 0.0008- 0.0020 ml per kg B.W per min.
For preparation of Lidocaine infusions, 1250 mg of Lidocaine hydrochloride (50 ml of 2.5% w/v Lidocaine Injection) may be added to 500 ml of appropriate glucose or sodium chloride infusion solutions. A 70 kg patient is to receive 0.8 – 1.6 ml of such infusion per min, corresponding to 2-4 mg Lidocaine hydrochloride per min.
As a general rule, the dosage should be guided by the individual requirements and the therapeutic effect.
The dose should be reduced in patients with heart failure, liver diseases, in patients receiving drugs which enhance the effects of Lidocaine, during pregnancy, and in patients who are more than 60 years old.
Renal insufficiency, as a rule, does not require specific dose adjustment. However, such patients should be monitored for toxic effects caused by accumulation of efficacious metabolites.
Children:
The safety and the efficacy of the use of Lidocaine in children have not been sufficiently established. The American Heart
Association, in their Standards and Guidelines for Cardio-pulmonary Resuscitation and Emergency Cardiology of 1985, recommend an initial dose of 1 mg/kg BW and subsequently, if required, infusion of 20 - 50 μg/kg BW/min. For ensuring sufficiently high plasma levels of Lidocaine, a second dose of 1 mg/kg BW may be injected prior to infusion.
2.Possible side effects
Frequently, especially under too rapid administration, central nervous disorders are observed, such as sleepiness, dizziness, vertigo, confusion, blurred vision, dysarthria, dysphagia, tinnitus, trembling, flushing, chills, tingling and skin paraesthesia, further restlessness, irritability, euphoria, hallucinations and depression. Frequently observed gastro-intestinal disorders include anorexia, nausea, and vomiting. These adverse effects are more frequent under rapid onset of systemic effects of lidocaine hydrochloride.
If undesirable effects are observed, the rate of administration of lidocaine must be reduced or administration must be discontinued.
Rarely, neurological complications following central nervous blocks – mainly spinal anaesthesia – may occur such as persistent anaesthesia, paraesthesia, paresis or plegia of the lower extremities and loss of sphincter control (e.g.cauda equina syndrome).
After spinal anaesthesia, transient pain in the lower extremities and lower back pain is commonly observed. The pain may last several (up to 5) days and will resolve spontaneously.
Proarrhythmic effects becoming manifest as alterations or aggravation of the originally present arrhythmia may lead to severe impairment of cardiac action possibly followed by cardiac arrest.
Rarely, especially in cases of overdosage, serious adverse effects such as muscular convulsions, possibly up to spasms of the entire body, impaired consciousness up to coma, respiratory depression or even arrest, drop of blood pressure, bradycardia, tachyarrhythmia and shock are observed.
Foetal bradycardia in connection with the use of lidocaine hydrochloride in obstetrics has been reported.
Allergic reactions such as exanthema, urticaria, oedema, hypotension and anaphylactic shock have been observed sporadically.
In elderly patients the incidence of side effects may be increased.
INGREDIENTS
Contents of the pack and other information
What Lidocaine Injection contains
•The active substance is lidocaine hydrochloride. Each ml contains 25 mg of lidocaine hydrochloride.
What Lidocaine Injection looks like and contents of the pack
•Lidocaine injection is a clear, sterile, nonpyrogenic solution, free from visible particles. It is supplied in a 50-mL glass vial.
•Pack size:
1 vial per carton.
STORE
How to store Lidocaine Injection
Keep this medicine out of the sight and reach of children.
Store at temperature not exceeding 25°C. Do not refrigerate or freeze.
Keep the ampoules in the outer carton until time of use in order to protect from light.
Do not use this medicine after the expiry date ‘EXP’ shown on the container. The expiry date refers to the last day of that month.
Do not throw away any medicines via wastewater or household. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.